 What To Know About A Dead Tooth
What To Know About A Dead Tooth
What is a dead tooth?
A dead tooth is a commonly used phrase for a tooth that has lost its blood flow and nerve function. Other terms for this condition include non-vital, pulpless, or necrotic teeth.
What causes it?
A dead tooth can occur whenever the tooth pulp becomes compromised.
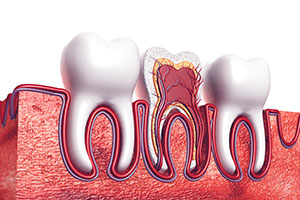
The structure of a tooth is made up of three distinct layers: enamel, dentin, and pulp. Enamel, the outermost layer, provides strength when chewing and resistance against cavities. Dentin is a softer material that makes up the bulk of the tooth structure. Finally, the pulp is the innermost layer, which consists of nerves and blood vessels.
Anytime a tooth suffers a traumatic injury, fracture, infection, or tooth decay, there is potential for pulp damage.
What are the symptoms?
The main symptoms of a dead tooth are discoloration and pain.
After an injury or infection occurs, there may be a period in which the tooth appears unaffected. However, as the nerve is dead or dying, pain may range from mild discomfort to severe distress. It can be either throbbing, a constant ache, or come and go periodically.
Even though it may sound contradictory to experience pain when the nerve is dead, it is often the surrounding nerves around the tooth that are signaling the problem.
Additionally, tooth color may darken slightly as the internal nerves and arteries decay.
What can be done to treat the condition?
For a painful tooth, the typical treatment involves a root canal. We access the infected tooth and remove any decayed matter. Then, a biocompatible material is used to fill the tooth. And finally (if necessary) we use a dental crown to provide strength and support.
When discoloration of the tooth has occurred, we may use internal whitening to help match the surrounding teeth. The whitening solution is placed inside the tooth, lightening the color at the source of the problem.
What else can happen?
If left untreated, a dead tooth can eventually result in tooth loss or spread of the infection. Surrounding teeth may be infected, or an abscess (pocket of infection) may form inside the gums.
Instead of allowing this to happen, it’s vital to schedule an appointment so we can evaluate your condition and provide a proper diagnosis. It is usually necessary to take X-rays to confirm suspicions of a dead tooth. Contact us today!





Comments are closed.